More notes from the Field: The role of leaders in sustaining and spreading improvement
In my post on 3 April, I showed a stair-step picture of improvement. The base of the stairs corresponds to developing a change. The next steps are testing, implementing, sustaining and spreading. I pointed out my failure in past consulting work to clearly indicate the role of managers and executive leaders in owning the Plan-Do-Study-Act cycles related to the upper steps, sustaining and spreading changes.
Last week, I got yet more evidence of the need to clarify jobs in improvement depending on the stage of work.
The Improvement Opportunity
A primary care medical practice has worked to increase the number of advance directives that its patients develop and are recorded in the practice’s electronic medical record system. The practice is part of a larger learning community. The learning community aims to help health care organizations improve the way they engage with their patients around what matters most in their care, especially at end of life.
Leaders at the practice identified one group of patients to start the improvement: patients coming for annual Medicare Wellness visits. The nurse in charge of these visits enthusiastically dove in. She tested a series of changes in the interaction she had with her patients, all with the aim of increasing the number of advance directives in the practice electronic record system.
She actually succeeded; over four months, working with monthly batches of patients, she raised the number of advance directives in the practice record system from under 10% to over 50%.
I checked in with the nurse the beginning of March about next steps in the practice. She felt optimistic about progress. She had ideas about sustaining the gains with the Medicare Wellness program, improving flow of information from patients who wished to use an electronic portal to communicate their advance directives. She also said providers were talking about extending the advance directives work to adult patients coming in for annual physical exams other than the Medicare Wellness visits.
When I checked in with the nurse again last week, I learned the pace of change and improvement had slowed. The senior managers were not yet ready to run their own PDSA cycles to sustain the initial changes and spread the work to engage more patients.
Why? Our improvement program has not insisted that the senior managers learn and practice Plan-Do-Study-Act along with their nurse. It’s as if we coached only the first and second runners on a track relay team in proper baton hand-offs and running techniques. From that perspective, we shouldn’t be surprised when the relay team doesn’t run swiftly across all the legs of the relay.
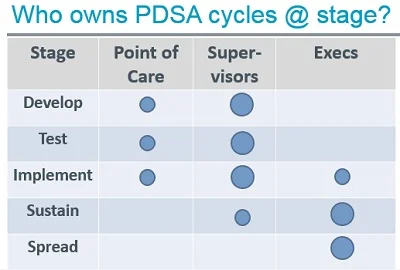
My conversations with the nurse led me to draft the table sketched at left. The size of the circles suggests frequency of ownership—e.g. in testing a change in a value stream or production process, the people who do the work sometimes own PDSA cycles but supervisors will own proportionally more of the cycles.
The table needs refinement through application. However, it seems good enough as a starting point for my work with executive sponsors of improvement projects. It gives me a chance to frame a conversation about roles and responsibilities in improvement. I tried it out last week on an introductory phone call with four organizations seeking to improve care of patients with rheumatoid arthritis; I’ll see if I can promote more effective PDSA by the leaders who have chartered those improvement efforts.